Autism, often misunderstood and misdiagnosed, is a complex neurological condition that shares overlapping traits with many mental health disorders. Unfortunately, this leads to a frequent misidentification of autism in adults. With symptoms mistakenly attributed to conditions like anxiety, depression, ADHD, bipolar disorder or personality disorders, many adults find themselves lost in a sea of labels. Autism presents itself differently in adults, especially in women. The limited awareness of how these traits manifest in individuals who might not fit the stereotypical image of autism can be highly damaging, leaving many people with a lack of clarity.
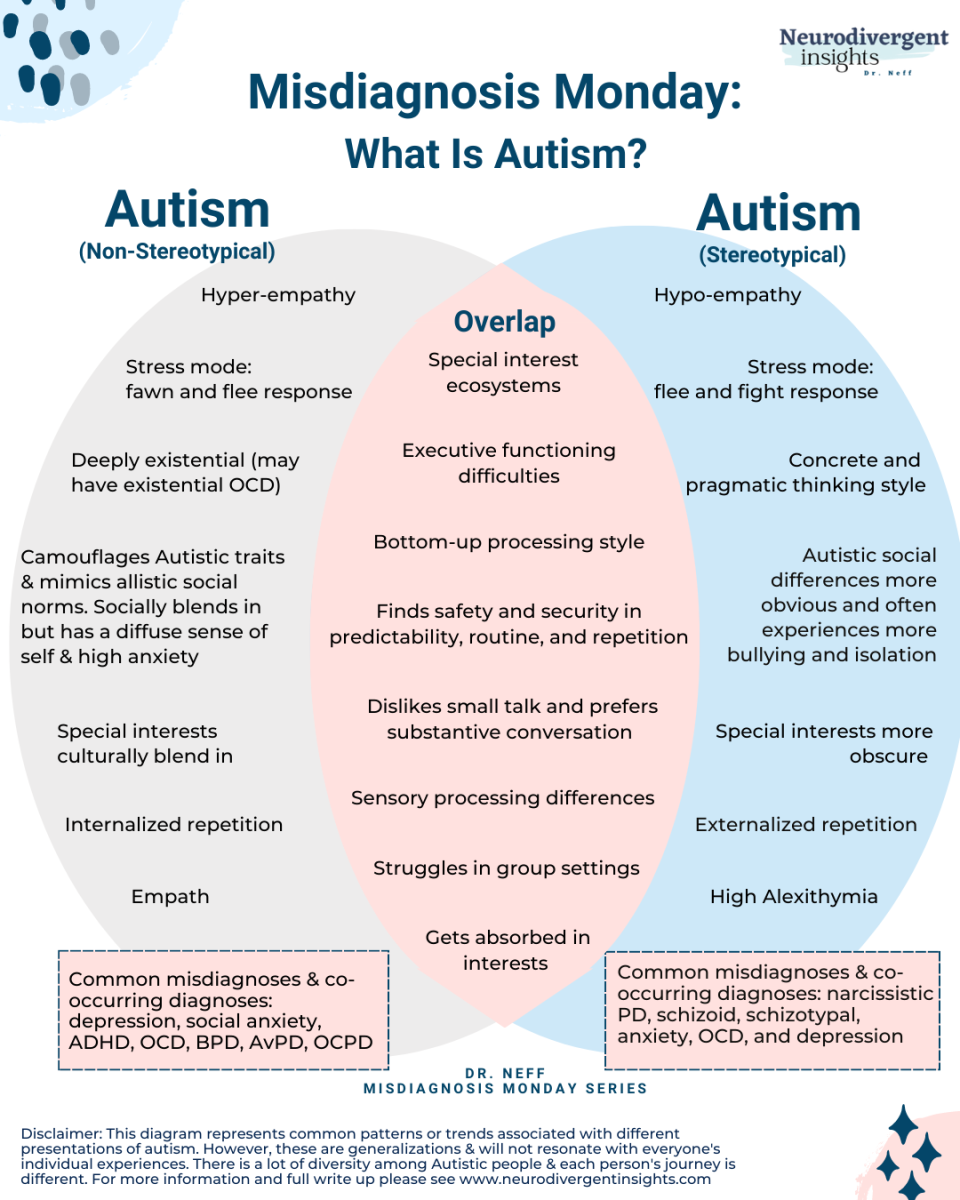
One of the most significant challenges in diagnosing autism is the overlap of its traits with those of other psychiatric conditions. For example, repetitive behaviors in autism can resemble the compulsions seen in obsessive-compulsive disorder (OCD). In addition, social withdrawal and difficulty navigating social interactions might be mistaken for social anxiety or depression. The complexity of autism’s physical presentation, combined with a lack of awareness about its diversity, makes accurate diagnosis all the more difficult.
In a study conducted by the National Autism Society, another critical factor contributing to misdiagnosis is masking. Extremely common in autistic women, masking is a behavior where individuals consciously suppress their autistic traits in order to fit in socially. It can be a learned coping mechanism, but it often makes it harder for clinicians to spot high-functioning autism. Individuals that exhibit milder symptoms and portray above average intelligence along with advanced verbal skills while still having sensory sensitivities are often seen as high-functioning neurodivergent individuals. With these signs clouding a clear diagnosis, the result is often a diagnosis of another condition, such as anxiety or mood disorders, when, in reality, the person has camouflaged autism.
Gender biases in autism diagnosis play a crucial role. Research shows that women are more likely to be misdiagnosed with mood disorders, anxiety disorders or personality disorders before psychologists correctly identify them as autistic. A study conducted by the National Institutes of Health revealed that 31.7% of autistic women report being misdiagnosed, compared to just 16.7% of men. This highlights the need for greater gender-sensitive approaches during mental analysis. The ways autism manifests in women can be significantly different from its presentation in men.
Clinicians often misinterpret autism as borderline personality disorder (BPD) due to emotional dysregulation, difficulty in relationship management, and instability in mood and behavior. Attributions of emotional regulation struggles and social withdrawal in autism to depression or generalized anxiety disorder often overlook the broader context of autism. With many overlapping symptoms such as inattention, hyperactivity and impulsivity, ADHD becomes the forefront for a diagnosis, leading clinicians to overlook the full spectrum of autistic behaviors.
These misdiagnoses have serious consequences for individuals with autism. Inappropriate treatments are a common outcome, where therapy may target the wrong condition or medications may exacerbate symptoms. For example, individuals misdiagnosed with depression may take prescribed antidepressants, which can be ineffective or even harmful for someone with autism. Similarly, therapy exclusive to another condition may overlook the unique needs of the autistic person.
Misdiagnosis often means that the individual does not receive the appropriate accommodations needed to manage their autism, which can prolong functional difficulties and emotional distress. Misunderstandings and ineffective treatments can also lead to a loss of self-esteem, increasing feelings of frustration and isolation.
According to the National Library of Medicine, clinicians should thoroughly evaluate an individual’s developmental history to address these issues. By looking beyond surface-level symptoms, professionals will become more adaptable in recognizing symptoms of autism, especially when symptoms overlap with other psychiatric conditions. Educating clinicians on these diverse presentations can help prevent misinterpretation.
Addressing this issue requires changes in diagnostic practices and increased awareness among healthcare professionals. With a deeper understanding and a more refined approach, individuals with autism can receive the recognition and support needed to lead healthy lives.